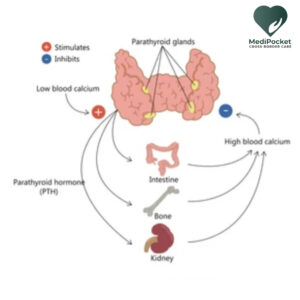
Primary hyperparathyroidism (PHPT) is a medical illness defined by an excess of parathyroid hormone (PTH) produced by one or more of the parathyroid glands, resulting in excessively high calcium levels in the blood (hypercalcemia). The parathyroid glands are four tiny glands in the neck that generate PTH, which aids in the regulation of calcium and phosphorus levels in the body.
What is hyperparathyroidism?
Hyperparathyroidism is a medical disorder that develops when the parathyroid glands (four tiny glands situated in the neck) create an excessive amount of parathyroid hormone (PTH). This might result in a rise in blood calcium levels, which can cause a number of symptoms and health concerns, such as bone loss, kidney stones, and gastrointestinal issues.
The most prevalent cause of hypercalcemia in adults is PHPT, which is caused by a non-cancerous growth, or adenoma, on one of the parathyroid glands. PHPT is less usually caused by multiple parathyroid gland hyperplasia or, in rare situations, parathyroid malignancy.
What is hypercalcemia?
Hypercalcemia is a medical disorder defined by unusually high calcium levels in the blood. Calcium is a mineral that is needed for many body activities, including bone health, neuron and muscle function, and blood coagulation.
Hypercalcemia is usually caused by an underlying medical condition such as primary hyperparathyroidism, some malignancies (such as multiple myeloma or lung cancer), or renal disease. Some drugs, such as thiazide diuretics or lithium, might also induce it.
Symptoms of primary hyperparathyroidism
PHPT is frequently asymptomatic, which means that many people with the disorder may not have any obvious symptoms. When symptoms do appear, they might range in severity and may include:
Fatigue and weakness: Individuals with PHPT may feel fatigued or weak, and they may struggle to do daily duties.
Bone pain and fractures: Excessive calcium levels in the blood can cause bones to become weaker and more brittle, resulting in bone pain, fractures, and osteoporosis.
Kidney stones: PHPT can cause calcium to build up in the kidneys, resulting in painful kidney stones.
Increased urination: Individuals who have PHPT may need to pee more frequently than normal and may be thirsty.
Constipation and abdominal discomfort: Excessive calcium levels can produce gastrointestinal symptoms such as stomach pain, constipation, and nausea.
Depression and anxiety: Some PHPT patients may experience mood swings such as sadness, anxiety, and irritability.
Memory loss and difficulties concentrating: PHPT can impair cognitive function, resulting in memory and concentration issues.
Untreated PHPT can cause major problems such as osteoporosis, renal damage, and pancreatitis in extreme instances. If you have any of these symptoms, you should seek medical attention for assessment and diagnosis.
Causes
Primary hyperparathyroidism (PHPT) is caused by an excess of parathyroid hormone (PTH) produced by one or more of the parathyroid glands in the neck. The precise aetiology of PHPT is not always evident, however there are a number of variables that might contribute to its spread.
Adenoma
A benign growth termed an adenoma that forms in one of the parathyroid glands is the most prevalent cause of PHPT. This tumor causes the gland to release an excessive amount of PTH, resulting in hypercalcemia (high levels of calcium in the blood) and PHPT symptoms.
Hyperplasia
PHPT is less usually caused by hyperplasia (enlargement) of one or more parathyroid glands. In this scenario, all of the glands overproduce PTH, resulting in hypercalcemia.
Carcinoma
PHPT can be induced in rare situations by a parathyroid carcinoma, a malignant tumor that creates an excess of PTH. Parathyroid cancer is exceedingly uncommon, accounting for fewer than 1% of PHPT occurrences.
Genetic mutations
Primary hyperparathyroidism risk can also be increased by some genetic mutations. Those with multiple endocrine neoplasia type 1 (MEN1) or type 2A (MEN2A), for example, are more likely to develop PHPT and other endocrine tumors.
Medications
Lastly, some drugs and medical circumstances can result in secondary hyperparathyroidism, which is a different illness defined by an increase in PTH synthesis in response to low calcium levels in the blood. Secondary hyperparathyroidism can evolve to PHPT if left untreated.
Diagnosis of primary hyperparathyroidism
Primary hyperparathyroidism is normally diagnosed using a combination of medical history, physical exam, and laboratory testing, such as:
Blood test: Blood tests can detect calcium, phosphorus, PTH, and other hormones that influence calcium levels in the blood.
Urine testing: Urine tests can detect calcium and other chemicals that suggest parathyroid gland disorders.
Imaging techniques, such as ultrasound, CT scan, or MRI, can aid in the detection of enlarged or atypical parathyroid glands.
Bone density scan: A bone density scan can detect whether hyperparathyroidism has resulted in bone loss, which can lead to osteoporosis.
If primary hyperparathyroidism is suspected, the diagnosis is confirmed by elevated levels of PTH and calcium in the blood, and other laboratory tests. Once the diagnosis is confirmed, further imaging tests may be performed to locate the specific gland(s) causing the problem.
Treatment
The therapy for primary hyperparathyroidism is determined by the severity of the ailment, the patient’s age and overall health, and the presence or absence of symptoms.
- Observation: In certain circumstances, especially when the patient has no symptoms, a “watch and wait” strategy with regular monitoring of calcium levels in the blood and bone density tests may be indicated.
- Surgery: Surgery is the most frequent therapy for primary hyperparathyroidism, and it is often suggested if the patient is suffering symptoms or consequences from the illness, or if the calcium levels in the blood are extremely high. The procedure is known as a parathyroidectomy, and it may be performed using minimally invasive procedures that need a smaller incision and less time.
- Medications: While some drugs can help reduce blood calcium levels, they are not normally used as the primary therapy for primary hyperparathyroidism. They may be utilized in exceptional circumstances, such as when surgery is not possible owing to medical concerns.
After surgery, the patient may need to take calcium and vitamin D supplements for a while to allow the remaining parathyroid glands to acclimatise to the shift in hormone production. Frequent check-ups and blood tests are also required to monitor calcium levels and ensure that the disease does not reoccur.
Generally, early detection and treatment of primary hyperparathyroidism are critical for avoiding long-term consequences like osteoporosis and kidney stones. Therapy can enhance the patient’s quality of life while also lowering the chance of major health issues.
Every year, this endocrine condition affects over 100,000 people, the majority of them are postmenopausal women. Although primary hyperparathyroidism cannot be avoided, symptoms can be reduced if treated early. It is advantageous to be on the lookout for potential indicators of the disease in order to obtain an early diagnosis.
Treatment from the United states
Do you know that the professionals in the United States are the finest at treating endocrine diseases? When it comes to diagnosis and treatment, their knowledge and years of devotion in the medical sector speak volumes. We also want Indians who cannot go all the way to America to have the greatest care available. No worries because MediPocket world is here to help. Bringing sustainable healthcare all the way from the US virtually to the Indian patients is our job. For the first time, people from India can get to talk to the American-board certified specialist for second opinion, USA treatment and clinical trials. Register and get connected with the best endocrinologist now.