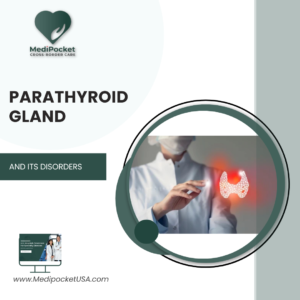
Neuropathy, also known as Peripheral Neuropathy, is a condition that affects the nerves that transmit information from the brain and spinal cord to the rest of the body. It occurs when these nerves are damaged or dysfunctional, which can result in a variety of symptoms depending on the severity and location of the damage.
Physical injury, infection, toxin exposure, chronic diseases such as diabetes or autoimmune disorders, and genetic predisposition can all lead to neuropathy. Age, alcohol abuse, and vitamin deficiencies are also risk factors for neuropathy.
Symptoms of Peripheral Neuropathy
Peripheral Neuropathy can cause a variety of symptoms, which vary depending on the type and severity of the condition. Some of the most common symptoms of peripheral neuropathy are as follows:
- Numbness and tingling: Numbness or tingling is frequently the first sign of peripheral neuropathy. You may feel pins and needles, as well as numbness or tingling in your hands, feet, arms, or legs.
- Burning or shooting pain: Some people with peripheral neuropathy may experience a sharp, shooting pain that feels like an electric shock. Others may feel a throbbing or burning pain in the affected area.
- Muscle weakness: Peripheral neuropathy can cause muscle weakness, making everyday tasks like walking or picking up objects difficult.
- Touch sensitivity: Some people with peripheral neuropathy may have increased touch sensitivity, making even light pressure or touch painful.
- Coordination loss: Peripheral neuropathy can impair your balance and coordination, making walking and other physical activities difficult.
- Difficulties with fine motor skills: Peripheral neuropathy can make fine motor skills such as buttoning a shirt or writing difficult.
- Autonomic symptoms: Peripheral neuropathy can sometimes affect the autonomic nervous system, which regulates involuntary functions like blood pressure, heart rate, and digestion. This can result in symptoms like sweating, nausea, and constipation.
Risk factors
Some of the most common risk factors are as follows:
- Diabetes: Diabetes is one of the leading causes of peripheral neuropathy. Over time, high blood sugar levels can cause nerve damage, resulting in symptoms such as numbness, tingling, and pain in the feet and hands.
- Alcoholism: Chronic alcoholism can cause nerve damage and lead to peripheral neuropathy.
- Infections: Peripheral neuropathy can be caused by infections such as HIV, hepatitis C, and Lyme disease.
- Auto-immune disorders: Autoimmune diseases, such as rheumatoid arthritis, lupus, and Guillain-Barre syndrome, can all cause peripheral neuropathy.
- Vitamin deficiencies: Vitamin deficiencies, such as vitamin B12, can cause peripheral neuropathy.
- Toxin exposure: Toxins like heavy metals, certain medications, and chemicals can all cause peripheral neuropathy.
- Age: Although peripheral neuropathy can occur at any age, it is more common in older adults.
- Genetics: Peripheral neuropathy is hereditary, which means that it is passed down through families.
- Trauma: Physical injury or nerve trauma can result in peripheral neuropathy.
If you have one or more of these risk factors, talk to your doctor about ways to reduce your risk and prevent peripheral neuropathy. Regular check-ups and early detection can aid in the management of symptoms and the prevention of further nerve damage.
Types of Peripheral Neuropathy
Peripheral neuropathy is classified into several types, each with its own set of causes and symptoms. Some of the most common types of peripheral neuropathy are as follows:
- Diabetic Neuropathy: Diabetic neuropathy is the most common type of peripheral neuropathy that affects diabetics. Over time, high blood sugar levels can cause nerve damage, resulting in symptoms such as numbness, tingling, and pain in the feet and hands.
- Hereditary Neuropathy: Some types of peripheral neuropathy are hereditary, which means they are passed down through families. Charcot-Marie-Tooth disease and Friedreich’s ataxia are two examples.
- Idiopathic neuropathies: The cause of peripheral neuropathy is unknown in some cases. This is referred to as idiopathic neuropathy.
- Autoimmune neuropathies: Peripheral neuropathy can be caused by autoimmune disorders such as Guillain-Barre syndrome.
- Infectious neuropathies: Peripheral neuropathy can be caused by infections such as HIV, hepatitis C, and Lyme disease.
- Toxic Neuropathies: Toxic neuropathies are caused by exposure to toxins such as heavy metals, certain medications, and chemicals.
- Compression Neuropathies:Compression neuropathies occur when nerves are compressed or pinched by nearby structures, such as in carpal tunnel syndrome or cubital tunnel syndrome, resulting in peripheral neuropathy.
- Nutritional neuropathies: Vitamin deficiencies, such as vitamin B12, can cause peripheral neuropathy.
Diagnosis
Peripheral neuropathy is typically diagnosed through a combination of physical exams, medical history, and diagnostic tests. The following are some of the most common methods for diagnosing peripheral neuropathy:
Physical exam:
Your healthcare provider will look for signs of muscle weakness, numbness, or decreased reflexes during a physical exam. Your blood pressure and heart rate may also be checked.
Medical history:
Your healthcare provider will inquire about your medical history, which includes any previous illnesses or injuries, a family history of neuropathy, and any medications or supplements you are currently taking.
Nerve conduction studies:
These tests assess the speed and strength of electrical signals as they pass through your nerves. They can aid in the detection of nerve damage or dysfunction.
Electromyography (EMG):
It is a test that involves inserting thin needles into the muscles in order to measure electrical activity. EMG can assist in identifying muscle weakness or atrophy caused by nerve damage.
Imaging test:
Imaging tests, such as MRI or CT scans, can aid in the identification of structural issues or abnormalities that may be causing nerve damage.
Blood tests
Blood tests can help identify any underlying conditions that may be contributing to peripheral neuropathy, such as diabetes or vitamin deficiencies.
Treatment
Treatment for peripheral neuropathy is determined by the underlying cause as well as the severity of the symptoms. Some of the most common treatments for peripheral neuropathy are as follows:
Medications:
Pain relievers, antidepressants, and anticonvulsants are among the medications that can be used to manage the symptoms of peripheral neuropathy. These medications can help to alleviate pain, improve sleep, and alleviate other neuropathy symptoms.
Topical treatments:
To relieve pain and discomfort, topical creams or patches containing capsaicin, lidocaine, or other medications can be applied directly to the skin.
Physical therapy:
Physical therapy can help to improve muscle strength and coordination, as well as reduce muscle stiffness and improve overall mobility. It may also help to prevent further nerve damage.
Transcutaneous Electrical Nerve Stimulation (TENS) therapy:
TENS therapy involves the use of a small device that sends electrical impulses to the nerves via electrodes placed on the skin. This therapy can help with pain relief and nerve function.
Lifestyle:
Changes in lifestyle, such as eating a healthy diet, quitting smoking, and drinking less alcohol, can help to improve overall health and reduce the risk of further nerve damage.
Surgery:
Surgery may be required in some cases to relieve nerve pressure or to remove tumors or other growths that may be causing nerve damage.
Alternate therapies:
Alternative therapies, such as acupuncture, massage, or yoga, may provide relief from peripheral neuropathy symptoms for some people.
As a result, the article covers all aspects of peripheral neuropathy and its symptoms. It is always advisable to be aware of certain warning signs in order to avoid future consequences.
When it comes to neuropathy, people should seek a second opinion. Medical experts and professionals always advise getting a second opinion for any type of disease, and what is better than getting an opinion from the best doctors in the United States? This is possible with the help of MediPocket USA. When it comes to second opinions and USA treatment for patients all over the world, the cross border care service is the best. Register now to speak with the top experts on board.